Folinic Acid: The Unsung Hero for IACIRS Recovery
If you’ve ever felt worse when starting treatment—more brain fog, anxiety, insomnia, or even strange neurological symptoms—you might have been told it’s just “die-off.” And sometimes, it is. But what if those symptoms aren’t just the result of microbial death or detox overload? What if they’re signaling a deeper issue—one that’s easy to overlook but surprisingly common in IACIRS?
Let’s talk about transient cerebral folate deficiency (CFD)—and why folinic acid is becoming one of the most important tools in my treatment toolbox.
IACIRS and Mitochondrial Dysfunction: A Hidden Connection
Infection-Associated Chronic Inflammatory Response Syndrome (IACIRS) is a term we use to describe the fallout from complex immune dysfunction triggered by chronic infections, biotoxin exposure (like mold), and environmental stressors. One of the downstream consequences of IACIRS is mitochondrial dysfunction—and not in the abstract sense. We're talking about real, measurable energy deficits in the body’s cellular engines.
During flares or early phases of treatment, increased inflammation and oxidative stress cause damage to mitochondrial membranes, resulting in mitochondria that are especially sluggish. Oxygen utilization is impaired, ATP production drops, and additional oxidative stress ramps up. And when mitochondria falter, a cascade of systems begins to fail—including folate transport to the brain.
The Folate Transport Problem
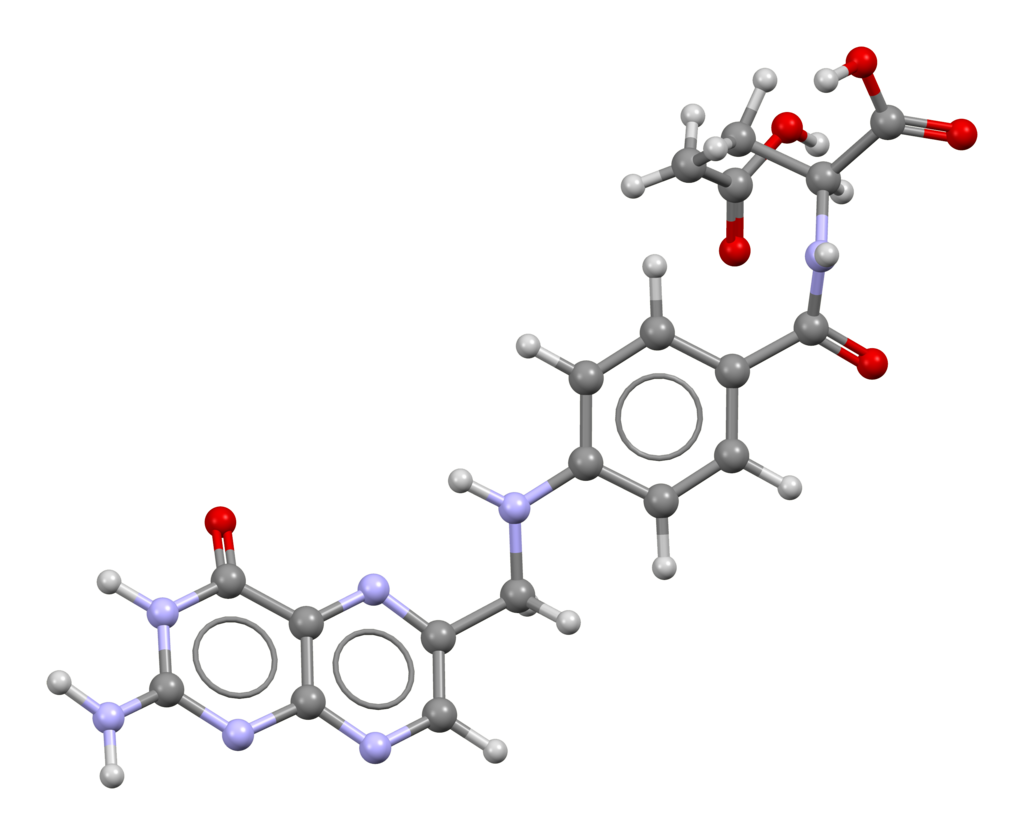
Your brain relies on a specialized folate receptor (folate receptor alpha) to import 5-methyltetrahydrofolate (5-MTHF)—the active form of folate commonly recommended for people with MTHFR mutations, especially C677T.
But here’s the problem: this receptor is energy dependent. It requires healthy mitochondrial function to do its job. And in people with IACIRS, especially during treatment flares or detox phases, mitochondrial output can drop—so folate transport slows or even halts.
The result? Cerebral folate deficiency (CFD)—not because you aren’t taking folate, but because it’s not getting into the brain.
In other cases, CFD may be caused by autoantibodies that block the folate receptor itself. These are called folate receptor alpha autoantibodies (FRAA), and they’ve been identified in both children and adults with neurological symptoms. FRAA can be tested using a blood panel called the FRAT (Folate Receptor Antibody Test).
But even when these antibodies are absent, mitochondrial dysfunction alone can impair folate transport by reducing the energy available for receptor function.
Symptoms of Cerebral Folate Deficiency (CFD)
CFD can mimic or worsen many of the symptoms already present in IACIRS. These include:
- Brain fog
- Fatigue
- Anxiety
- Insomnia
- Tics and other neurological movement disorders
- Irritability or mood swings
- Depression
- Poor stress tolerance
- Sensory processing issues
- Cognitive slowing or poor word recall
- Neuropathic pain or tingling
It’s no wonder that when folate transport gets disrupted, people feel like they’re backsliding—even when they’re on the right path.
The MTHFR Dilemma
Most people with a C677T MTHFR variant are told to take 5-MTHF—and for good reason. This is the form needed to optimize the methylation cycle, which is involved in detoxification, neurotransmitter synthesis, hormone regulation, and more.
(You can read more about this in my MTHFR blog.)
But here’s the catch: if 5-MTHF is the only form of folate you’re taking, and you can’t transport it into the brain due to mitochondrial dysfunction, then all that methylation support stops short—and CFD symptoms emerge or worsen.
So what’s the fix?
The Folate Workaround: Folinic Acid
Enter folinic acid (also known as calcium folinate). This is a different form of folate that does not rely on the folate receptor alpha to cross into the brain. It takes a separate, less energy-intensive pathway—and it works even when mitochondria are underperforming.
Once inside the central nervous system, folinic acid can still be converted into 5-MTHF, making it especially valuable for people with MTHFR variants who are experiencing signs of CFD.
More importantly, it provides a way to bypass the folate transport bottleneck that often shows up during IACIRS treatment.
How I Use It in Practice
More and more, I’m recommending folinic acid for patients who:
- Have had difficulty tolerating treatments
- Report ongoing neuropsychiatric symptoms despite treating root causes
- Experience die-off reactions that seem disproportionate
- Struggle with tics, OCD, or PANS/PANDAS-like presentations
In many cases, folinic acid has been the missing piece—quietly restoring folate flow to the brain, calming immune reactivity, and helping patients tolerate the very treatments that used to trigger setbacks.
It doesn’t work overnight, but it often shifts things meaningfully within a few weeks. And when layered in gently—alongside mitochondrial support and nervous system regulation—it can help stabilize the healing process for those who feel stuck.
That said, more is not always better. I often recommend starting with a very low dose (even 200 mcg or less), especially in sensitive patients. Going too high too quickly can actually increase agitation, irritability, or aggression in some people. It’s best layered in slowly and titrated to response—just like everything else in a thoughtful IACIRS protocol.
The Takeaway
Cerebral folate deficiency isn’t just a pediatric concern—it’s a real and under-recognized problem in adults with IACIRS, especially during phases of detox or infection treatment. If you’ve been told to take 5-MTHF but are still struggling with fatigue, insomnia, or mood symptoms, it might be time to consider a broader approach.
Folinic acid won’t fix everything. But it may be exactly what your brain has been missing.
References
- Ramaekers V, Rothenberg SP, et al. Folate receptor autoimmunity and cerebral folate deficiency.
- Quadros EV. Folate transport across the blood-brain barrier.
- Rossignol DA, Frye RE. Mitochondrial dysfunction in neurodevelopmental and neuropsychiatric disorders.
- Buescher AV et al. Elevated FIGlu as a biomarker for cerebral folate deficiency.
- Li X, et al. The impact of mitochondrial stress on folate metabolism.
- Delorme R, et al. Histamine pathways and folate-dependent methylation.
- Gupta S, et al. Clinical responses to folinic acid in chronic neuroinflammatory conditions.
- Image By Ben Mills - Own work, Public Domain, Link